The future prospects of cell
and gene therapy
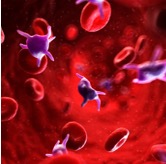
Hematological Disorder
Role of Cell and Gene Therapy in Hematological Disorder
- Sickle Cell Disease (SCD)
- Gene Therapy:
- Gene Addition: This approach involves inserting a functional copy of the beta-globin gene into hematopoietic stem cells (HSCs) to produce healthy red blood cells. Clinical trials using lentiviral vectors to deliver the functional gene have shown promising results, with patients experiencing increased levels of normal hemoglobin and reduced symptoms.
- Gene Editing: Technologies like CRISPR-Cas9 are used to correct the mutation in the HBB gene that causes SCD. Gene editing can either directly repair the mutation or reactivate fetal hemoglobin (HbF) production, which can compensate for the defective adult hemoglobin.
- Cell Therapy: Allogenic Hematopoietic Stem Cell Transplantation (HSCT) using stem cells from a matched donor, has been used as a curative treatment for SCD. The transplanted healthy stem cells can produce normal red blood cells, reducing or eliminating the symptoms of SCD. However, this approach is limited by the availability of suitable donors and the risk of graft-versus-host disease (GVHD).
- Gene Therapy:
- Beta-Thalassemia
- Gene Therapy:
- Gene Addition: Similar to SCD, beta-thalassemia can be treated by adding a functional beta-globin gene to HSCs using lentiviral vectors. Clinical trials have demonstrated that this approach can reduce or eliminate the need for blood transfusions in patients with transfusion-dependent beta-thalassemia.
- Gene Editing: CRISPR-Cas9 and other gene-editing tools are being used to correct the mutations in the HBB gene or to reactivate HbF production. Early studies have shown promising results, with corrected cells producing normal levels of hemoglobin.
- Cell Therapy: Allogeneic HSCT from a matched sibling or unrelated donor can cure beta-thalassemia by providing a source of healthy HSCs capable of producing normal red blood cells. This treatment can significantly improve the quality of life for patients but is also limited by donor availability and the risk of GVHD.
- Gene Therapy:
- Hemophilia
- Gene Therapy: Gene therapy for hemophilia involves delivering genes that encode clotting factors VIII (for hemophilia A) or IX (for hemophilia B) to the liver or other target cells using viral vectors. Clinical trials have shown that a single administration of gene therapy can lead to sustained production of the clotting factor, reducing the need for regular infusions and improving bleeding control.
- Cell Therapy: Mesenchymal Stem Cells (MSCs) are being investigated for their potential to deliver clotting factor genes and promote tissue repair in hemophilia patients. While still in early stages, MSC therapy could provide a long-term solution for managing hemophilia.
- Leukemia
- Gene Therapy: Chimeric Antigen Receptor T-cell (CAR-T) Therapy involves engineering a patient’s own T cells to express receptors that recognize and attack leukemia cells. This approach has shown remarkable success in treating certain types of leukemia, such as acute lymphoblastic leukemia (ALL), leading to high remission rates.
- Cell Therapy: Allogeneic HSCT is a standard treatment for many types of leukemia. It involves transplanting healthy HSCs from a donor to replace the patient’s diseased bone marrow. This procedure can provide a long-term cure but carries risks, including GVHD and infection.
- Lymphoma
- Gene Therapy: CAR-T cells targeting CD19, a protein expressed on the surface of B-cell lymphomas, have shown significant efficacy in treating relapsed or refractory lymphomas. This therapy involves modifying the patient’s T cells to attack lymphoma cells, leading to durable remissions in many patients.
- Cell Therapy: Both autologous (using the patient’s own cells) and allogeneic HSCT are used to treat lymphomas. Autologous HSCT is often used after high-dose chemotherapy to restore the patient’s bone marrow, while allogeneic HSCT can provide a potential cure through the graft-versus-lymphoma effect.
