The future prospects of cell
and gene therapy
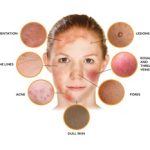
Skin Disorder
Role of Cell and Gene Therapy in Skin Disorder
- Epidermolysis Bullosa (EB)
- Gene Therapy:
- Gene Addition: EB is caused by mutations in genes encoding for proteins that provide structural integrity to the skin. Gene therapy aims to deliver functional copies of these genes, such as COL7A1 for dystrophic EB, to skin cells. This approach can restore the production of essential proteins and improve skin integrity.
- Ex Vivo Gene Therapy: In this method, patients’ keratinocytes (skin cells) are harvested, genetically corrected in the laboratory, and then re-transplanted onto the patient’s skin. Clinical trials have shown promising results, with improved skin stability and reduced blistering.
- Gene Therapy:
- Cell Therapy: Autologous keratinocyte transplantation involves harvesting the patient’s skin cells, expanding them in culture, and then grafting them back onto the patient. This technique can help replace damaged skin with healthy tissue.
- Vitiligo
- Gene Therapy: Gene therapy approaches for vitiligo focus on modulating the immune response to prevent the destruction of melanocytes, the cells responsible for skin pigmentation. Delivering genes that encode anti-inflammatory cytokines or immune regulatory proteins can help restore skin color.
- Cell Therapy: Transplanting cultured melanocytes into depigmented areas of the skin can restore pigmentation. This technique has shown success in repigmenting skin in vitiligo patients, particularly when combined with other therapies such as phototherapy.
- Psoriasis
- Gene Therapy: Psoriasis is characterized by an overactive immune response leading to excessive skin cell proliferation. Gene therapy can deliver genes encoding for anti-inflammatory cytokines, such as IL-10, to reduce inflammation and normalize skin cell growth.
- Cell Therapy: Mesenchymal Stem Cells (MSCs) have immunomodulatory properties that can help reduce inflammation and promote skin healing in psoriasis patients. Clinical studies have reported improvements in skin lesions and overall disease severity with MSC therapy.
- Cutaneous T-Cell Lymphoma (CTCL)
- Gene Therapy: Gene therapy can deliver therapeutic genes directly to the cancerous T cells in CTCL. For example, delivering genes that encode for tumor suppressor proteins or pro-apoptotic factors can induce cell death in the malignant cells.
- Cell Therapy: Chimeric antigen receptor T cells are engineered to target specific antigens expressed on CTCL cells. CAR-T cell therapy has shown promise in selectively attacking and eliminating cancerous T cells, leading to remission in some patients.
- Chronic Wounds
- Gene Therapy: Gene therapy can deliver genes encoding for growth factors such as VEGF (vascular endothelial growth factor) and PDGF (platelet-derived growth factor) to promote angiogenesis and tissue repair in chronic wounds. This approach can enhance wound healing by stimulating the formation of new blood vessels and tissue regeneration.
- Cell Therapy: Stem cells, including MSCs and adipose-derived stem cells, can be applied to chronic wounds to promote healing. These cells can differentiate into various cell types and secrete growth factors that enhance tissue repair and reduce inflammation.
