The future prospects of cell
and gene therapy
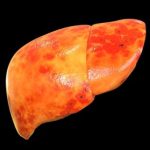
Liver Disease
Role of Cell and Gene Therapy in Liver Disease
- Inherited Metabolic Liver Diseases
- Gene Therapy:
- Wilson’s Disease: Wilson’s disease is caused by mutations in the ATP7B gene, leading to copper accumulation in the liver. Gene therapy using adeno-associated virus (AAV) vectors to deliver a functional ATP7B gene to liver cells can restore normal copper metabolism and prevent liver damage. Preclinical studies have shown promising results, with ongoing clinical trials to assess safety and efficacy.
- Glycogen Storage Diseases: These diseases, such as Pompe disease, are caused by enzyme deficiencies that lead to glycogen accumulation. Gene therapy can deliver genes encoding the missing enzymes, such as acid alpha-glucosidase (GAA) for Pompe disease, to liver cells, restoring normal metabolism and reducing symptoms.
- Acute Liver Failure
- Cell Therapy:
- Hepatocyte Transplantation: Transplanting healthy hepatocytes into patients with acute liver failure can provide a temporary bridge to liver transplantation or support liver regeneration. This approach has shown promise in preclinical models and early clinical studies, with transplanted hepatocytes integrating into the liver and performing necessary metabolic functions.
- Mesenchymal Stem Cells (MSCs): MSCs have immunomodulatory and regenerative properties that can help reduce inflammation and promote liver repair. Infusing MSCs into patients with acute liver failure has shown potential in reducing liver damage and improving liver function.
- Chronic Liver Disease and Cirrhosis
- Gene Therapy: Gene therapy approaches aim to deliver genes encoding antifibrotic proteins or cytokines to the liver to reduce fibrosis and promote tissue repair. For example, delivering genes that encode for matrix metalloproteinases (MMPs), which break down fibrotic tissue, can help reverse liver fibrosis in patients with chronic liver disease.
- Cell Therapy:
- Liver-Derived Progenitor Cells: These cells have the potential to differentiate into hepatocytes and other liver cell types, promoting liver regeneration and reducing fibrosis. Early-phase clinical trials are investigating the safety and efficacy of liver-derived progenitor cell transplantation in patients with cirrhosis.
- Bone Marrow-Derived Stem Cells: Bone marrow-derived stem cells can home to the liver and differentiate into hepatocyte-like cells, contributing to liver regeneration. Clinical studies have shown that these cells can improve liver function and reduce fibrosis in patients with cirrhosis.
- Hepatocellular Carcinoma (HCC)
- Gene Therapy:
- Oncolytic Viruses: These viruses are genetically engineered to selectively infect and kill cancer cells while sparing normal cells. Oncolytic virus therapy is being explored for HCC, with early-phase clinical trials showing promising results in reducing tumor size and improving survival.
- Tumor Suppressor Genes: Delivering genes that encode tumor suppressor proteins, such as p53, can inhibit cancer cell proliferation and induce apoptosis. Gene therapy targeting tumor suppressor pathways is being investigated as a potential treatment for HCC.
- Cell Therapy: Chimeric antigen receptor T cells are engineered to target specific antigens expressed on HCC cells. CAR-T cell therapy is being explored for its potential to selectively attack and kill liver cancer cells, providing a novel immunotherapeutic approach for HCC.
